Micromotion at the implant-abutment level has been identified as a major determinant of long-term implant success. Technical problems ranging from screw loosening to screw fracture may occur as a consequence of excessive micromotion. Different concepts for the design of the implant-abutment connection have been proposed in the past. These affect micromotion at the restorative interface as well as the stability of the abutments used.
While initial micromotion depends predominantly on the fabrication accuracy achieved, long-term micromotion appears to be related primarily to wear phenomena at the implant-abutment interface.
Despite the clinical importance of micromotion phenomena at the implant-abutment interface, no universally valid method for quantifying this phenomenon has been described.
Key point
It cannot be predicted that a certain type of abutment will always lead to a certain level of micromotion. Relative displacement of components occurs at varying magnitudes. However, strict adherence to manufacturers’ guidelines with respect to tightening torque may help reduce implant-abutment micromotion. Because micromovement occurs during the initial phase of loading, it may be prudent to routinely retighten the abutment screws, which might have lost preload.
Authors
Dr. Matthias Karl, department of prosthodontics, University of Erlangen-Nuremberg, Erlangen, Germany; Dr. Thomas D. Taylor, department of reconstructive sciences, University of Connecticut, Farmington, Conn.
Purpose
Scientists aimed to establish a bio-mechanical approach to directly measure relative motion at the implant-abutment interface and to quantify micromotion in a variety of implant-abutment combinations. Geometry of the implant-abutment interface, fabrication method of the abutment, engagement of antirotational features, abutment material, tightening torque and type of manufacturer (original, clone) were investigated.
Materials and methods
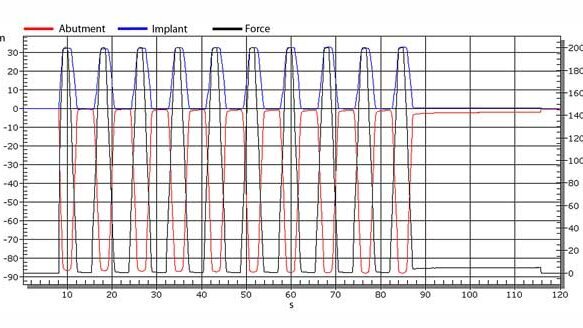
Implant-abutment assemblies were fixed in a universal testing machine at a 30-degree angle. A cyclic load of 200 N (Newtons) was applied to the specimens 10 times at a cross head speed of 100 N/s while relative displacement between the implant and the abutment was quantified using extensometers. For five consecutive loading cycles per specimen, micromotion was recorded as a basis for statistical analysis. Comparative analysis was based on Welch tests.
Results
Investigated implant-abutment combinations produced a broad range of micromotion values. Researchers did not find perfect implant shoulder geometry or perfect fabrication technique that would result in undetectable micromotion. The values for micromotion at the implant-abutment interface ranged from 1.52 to 94.00 µm (micrometers).
Researchers found tightening torque significantly affected the level of micromotion when one specific abutment type was investigated.
Implant shoulder design did not reveal a significant effect in all cases. Lack of engagement of antirotational features of the implants resulted in increased micromotion, regardless of the implant system investigated.
Casting onto prefabricated gold cylinders resulted in abutments with significantly less micromotion as compared to copy-milled stock abutments. Computer-aided design/computer-assisted manufacture (CAD/CAM) zirconia abutments showed less micromotion than CAD/CAM titanium abutments. Inconsistent levels of micromotion were recorded for CAD/CAM abutments coupled to proprietary and competing implant systems.
In most cases, the CAD/CAM abutments performed as well as stock abutments. Great variations in micromotion were found with clone abutments and clone implant systems.
More information
For a complete copy of the study and the JOMI November/December table of contents, visit www.osseo.org/NEWIJOMI.html. To join AO and begin receiving JOMI (bi-monthly) or obtain online access to JOMI, visit www.osseo.org/NEWmembershipApply.html.
This study was published in the November/December 2014 issue of The International Journal of Oral and Maxillofacial Implants (JOMI), the official journal of the Academy of Osseointegration (AO).
Background: Current implant protocols require not only osseointegration but also high levels of soft-tissue stability and esthetics. Crestal bone changes ...
The introduction of zirconia to the dental field opened the design and application limits of all-ceramic restorations. Thanks to its high strength and ...
SAN DIEGO, Calif., USA: Are you looking for ways to decrease chair time and emergencies with Class II corrections? If so, you might be interested in an ...
According to the American Association of Oral and Maxillofacial Surgeons, 69 percent of adults ages 35 to 44 have lost at least one permanent tooth to an ...
Implant dentistry is an expanding field. Ensure your skills are strengthened and that you can manage every appropriate phase of your implant care through a ...
NEW YORK, USA: Astra Tech, a provider of comprehensive solutions for dental implant therapy based in Waltham, MA, USA, recently announced the ...
LOUISVILLE, Ky., USA: Beam Technologies, a new enterprise in digital oral healthcare products, has developed the first toothbrush fitted with a Bluetooth ...
HOUSTON, Texas, USA: Accelerated orthodontic treatment will be a featured topic at the American Association of Orthodontics 2015 Annual Session, to be held ...
NEW YORK, NY /ALBUQUERQUE, NM, USA: OCO Biomedical has introduced 2.2- and 2.5-millimeter I-Micro dental implants. The implants are available in both crown ...
LOMA LINDA, Calif., USA: The indications and versatility of dental implants have increased, and so have complications. Researchers from the Loma Linda ...
Live webinar
Wed. 4 March 2026
8:30 PM EST (New York)
Lancette VanGuilder BS, RDH, PHEDH, CEAS, FADHA
Live webinar
Fri. 6 March 2026
3:00 AM EST (New York)
Live webinar
Mon. 9 March 2026
12:30 PM EST (New York)
Live webinar
Mon. 9 March 2026
3:00 PM EST (New York)
Live webinar
Tue. 10 March 2026
4:00 AM EST (New York)
Assoc. Prof. Aaron Davis, Prof. Sarah Baker
Live webinar
Tue. 10 March 2026
8:00 PM EST (New York)
Dr. Vasiliki Maseli DDS, MS, EdM
Live webinar
Wed. 11 March 2026
12:00 PM EST (New York)
MDT Andreas Chatzimpatzakis



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East



















































I’m interested in this article