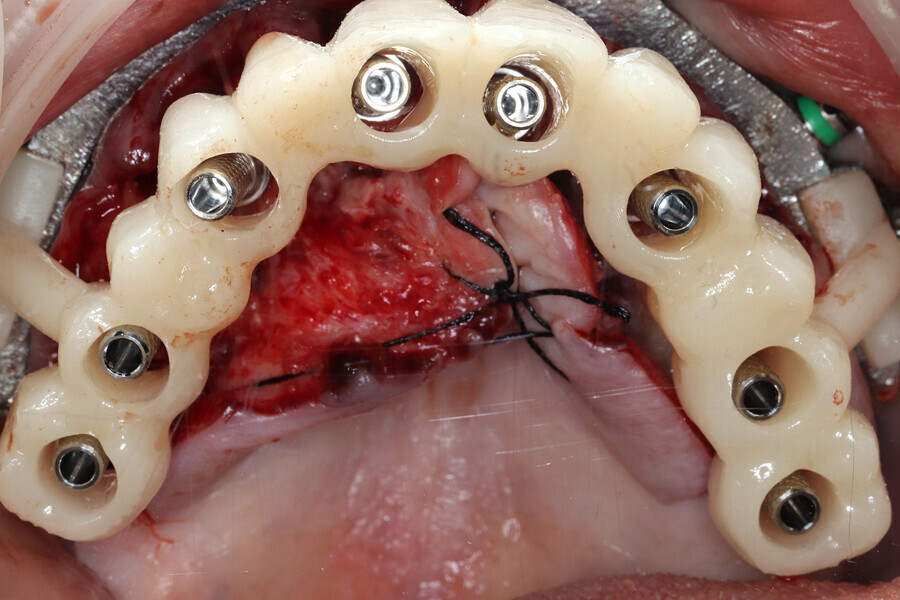
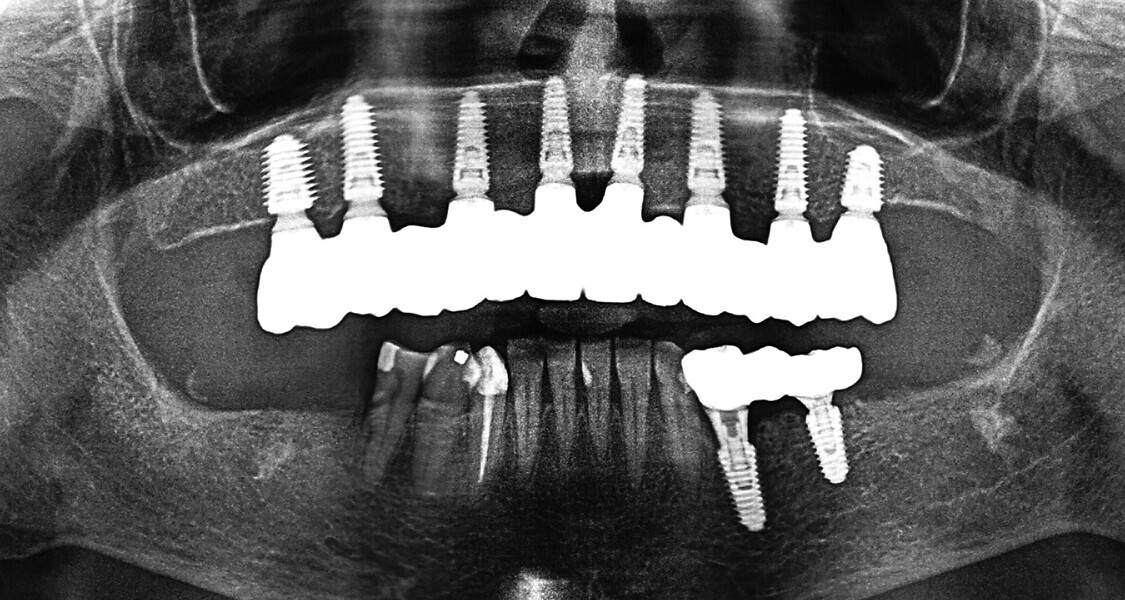
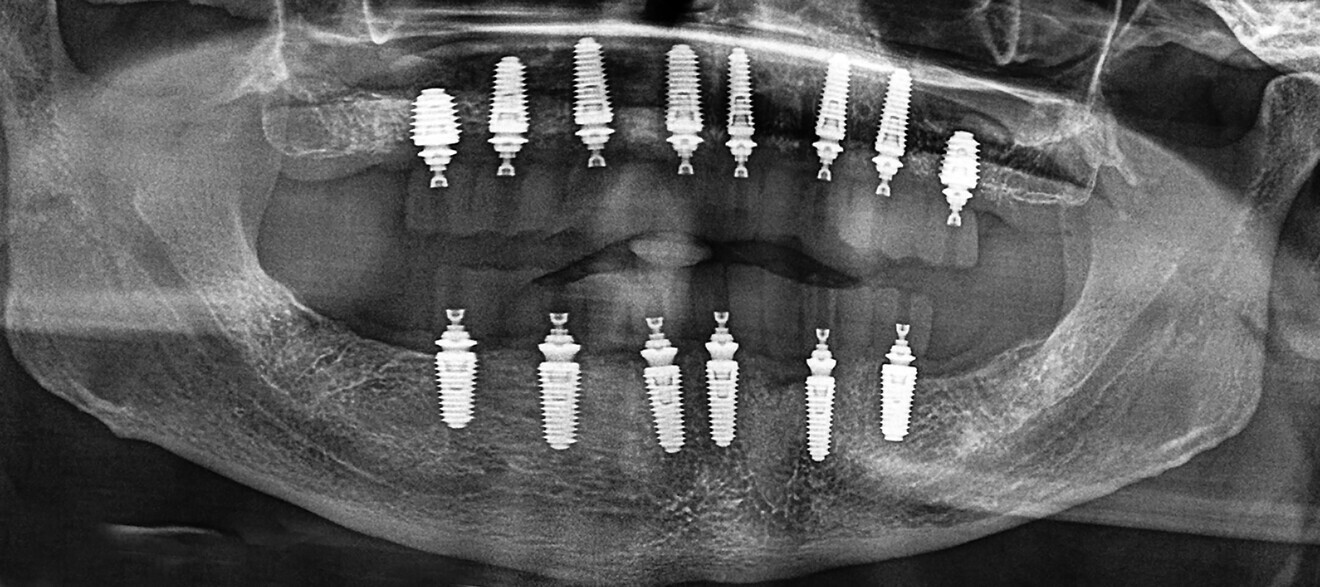
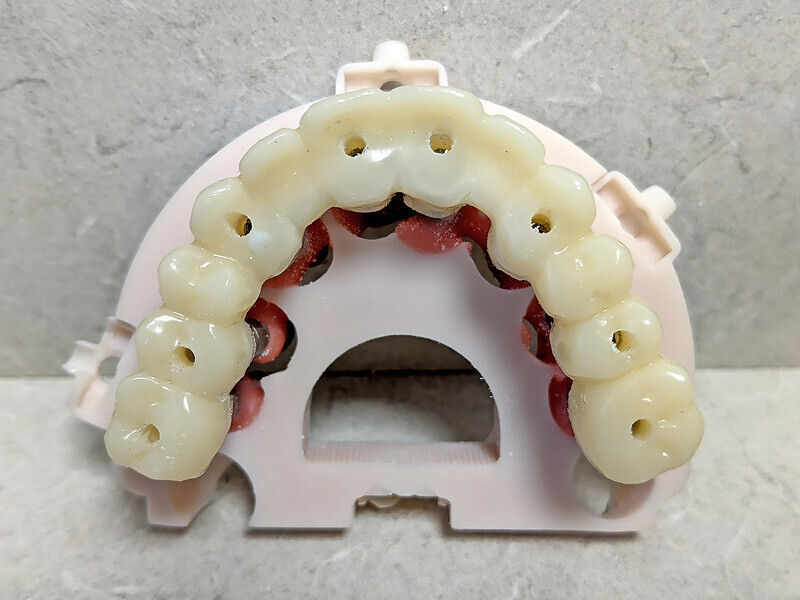
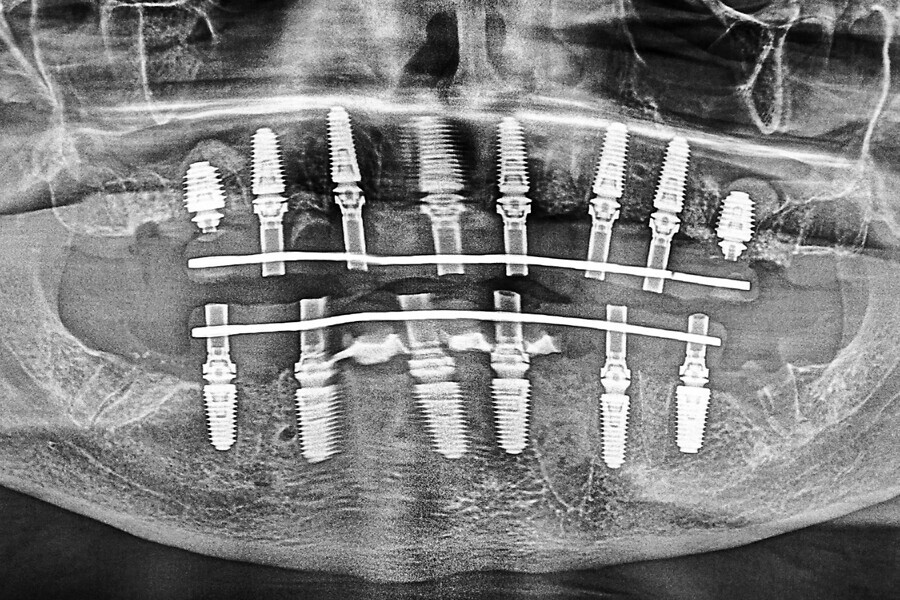
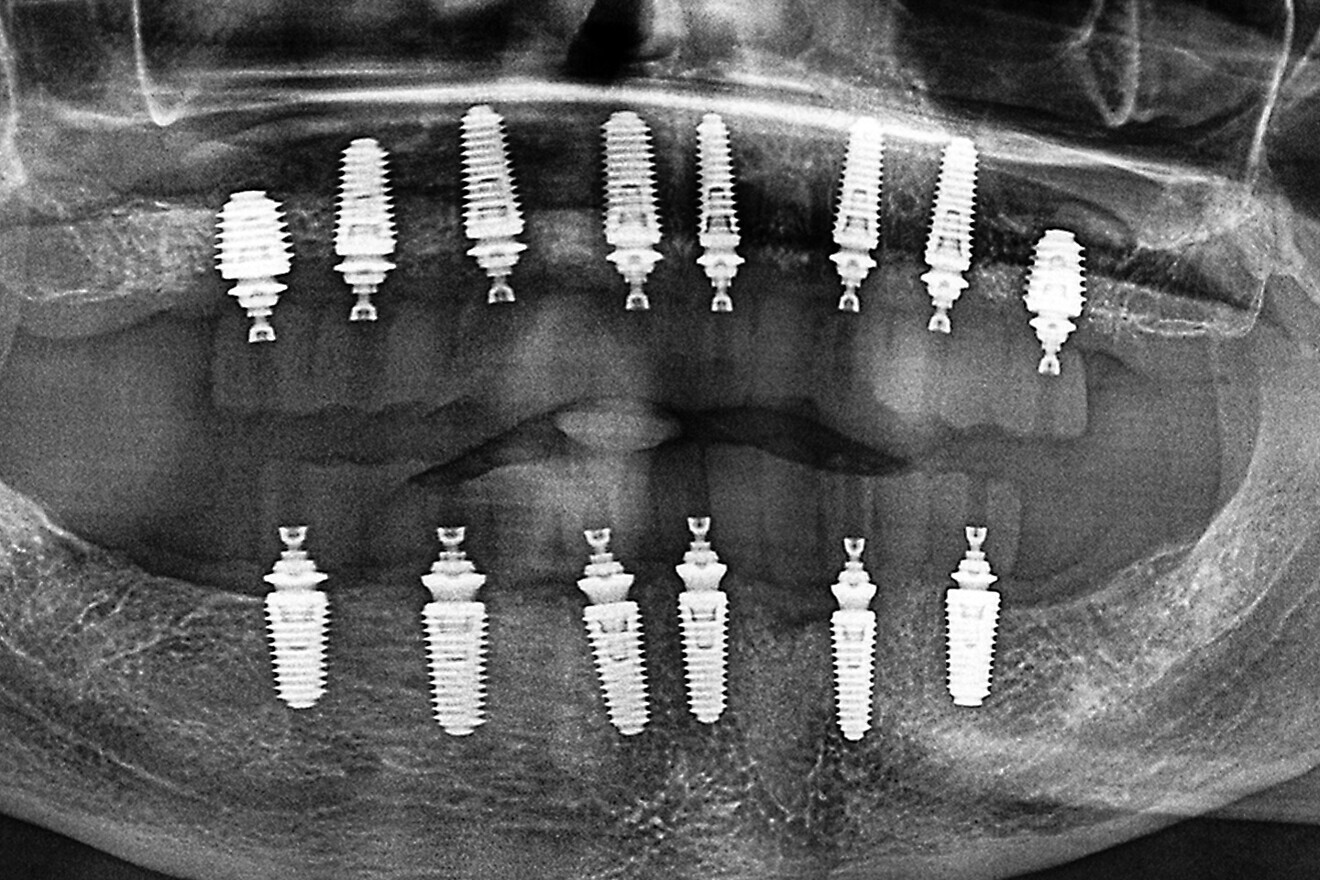
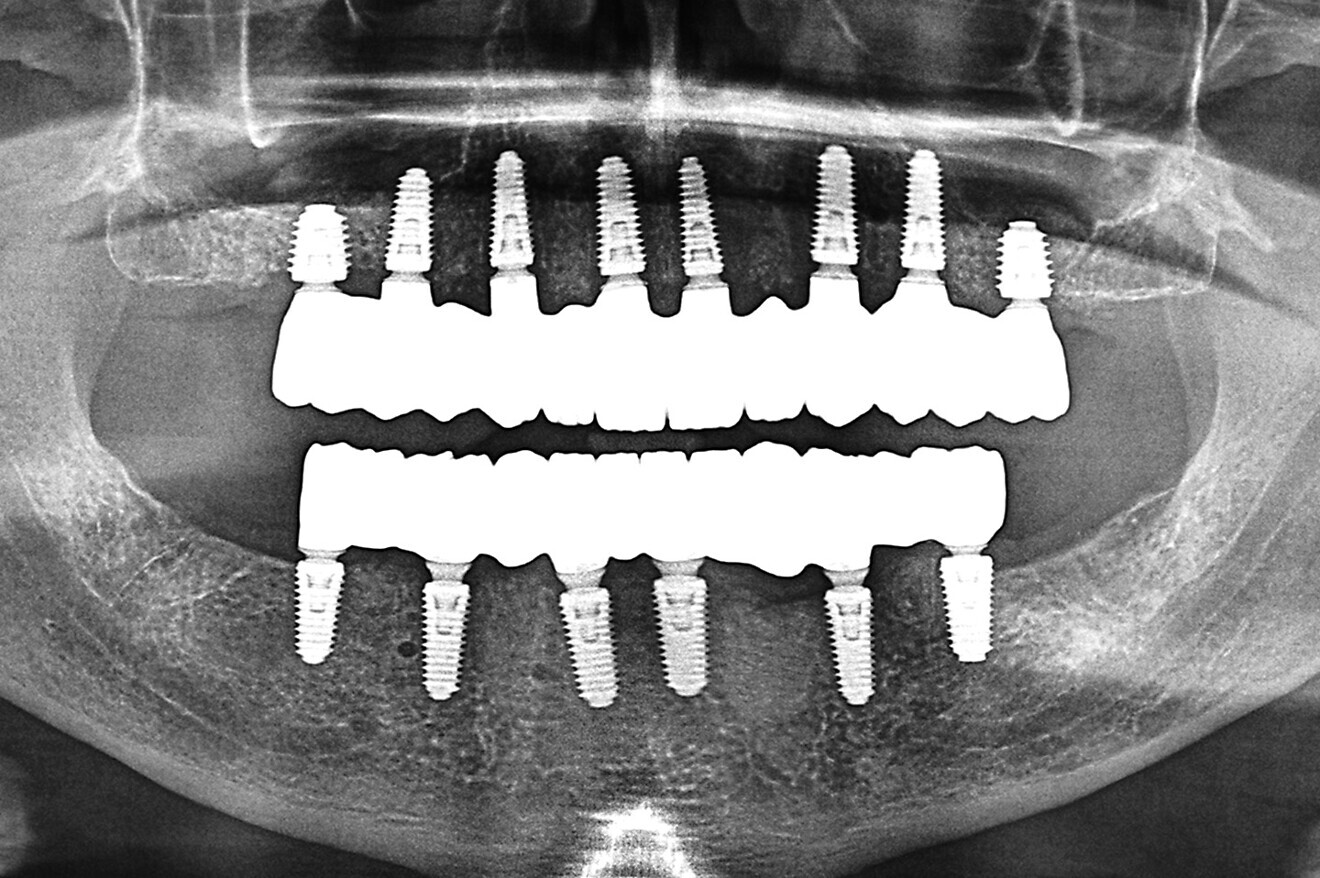
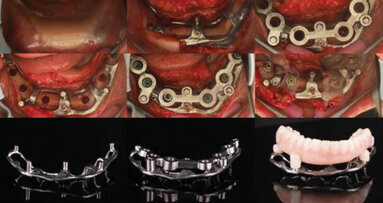
The final restorations were passively and accurately seated ten days later uneventfully using Vortex LA VIS screws. Confirmation records were taken with photographs, radiographs and digital articulation to recheck fit, function, phonetics and occlusion (Fig. 17a). The patient was extremely satisfied with his final restorations, describing the process as life-changing and surprisingly fast in comparison with what he had heard about full-mouth implant therapy. He was especially pleased with the speed at which the final process was able to be completed (Figs. 17b & c).
Conclusion
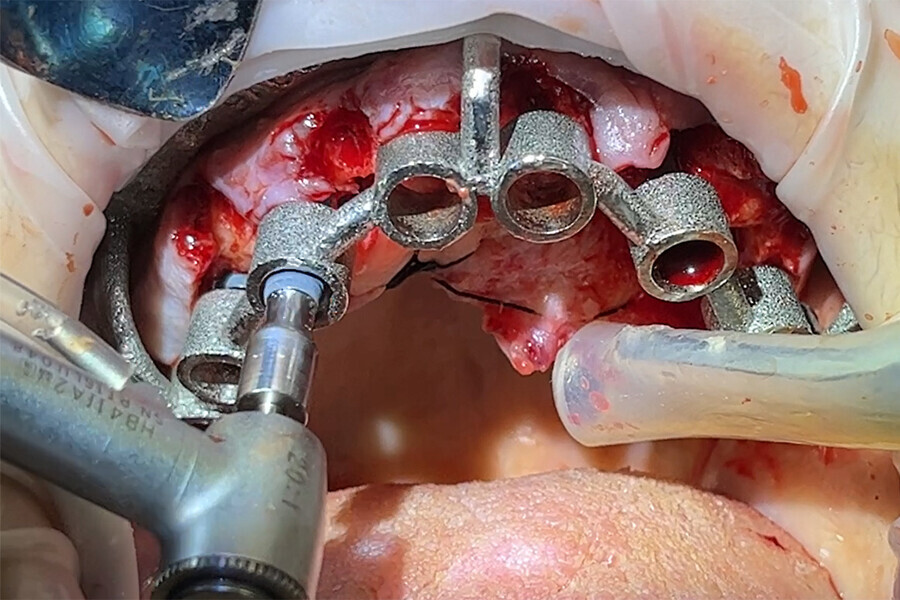
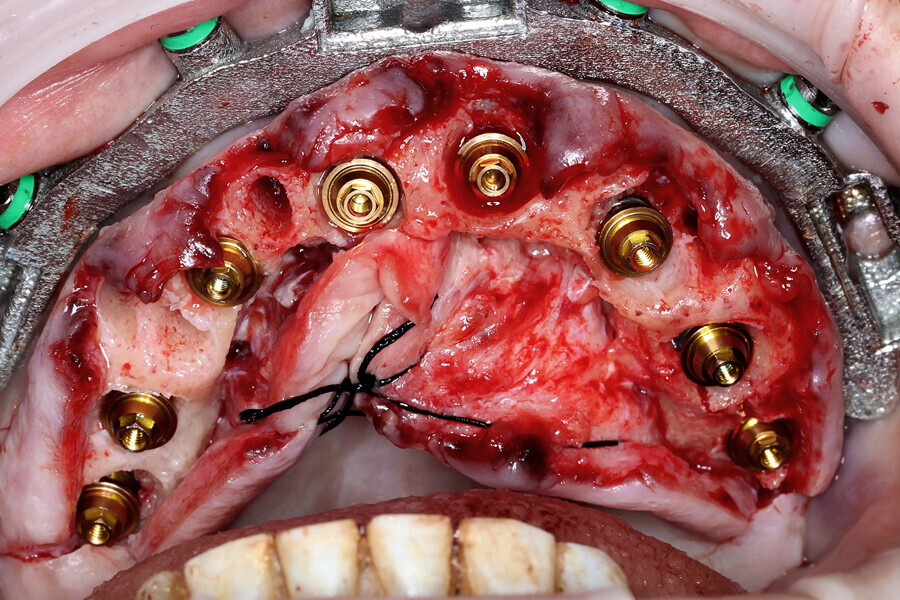
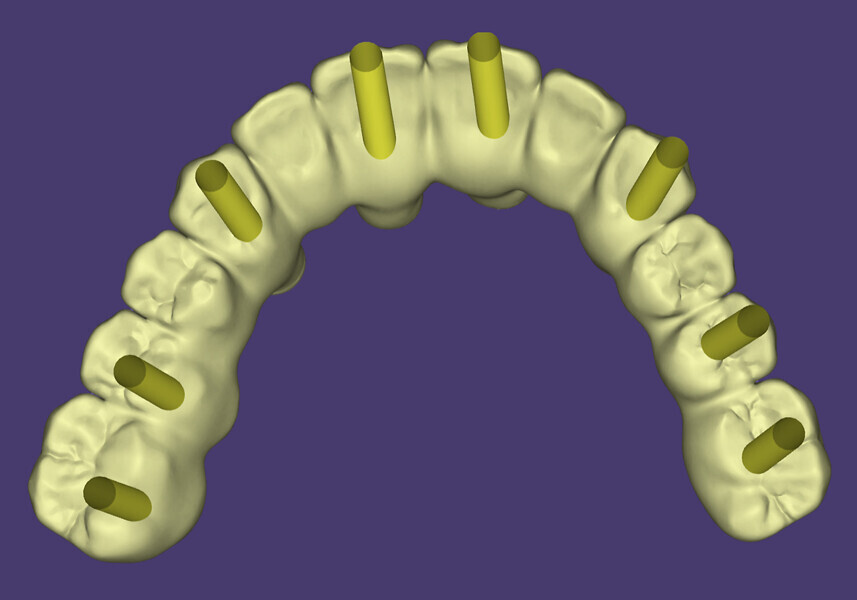
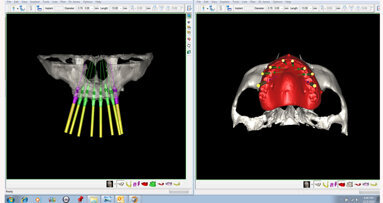
With proper diagnosis and treatment planning, single-arch or full-mouth implant reconstruction can be completed in a timely manner under ideal circumstances. The implementation of restoratively driven guided surgery can improve accuracy and ensure proper implant placement, including depth and angulation. Data collection at either the time of surgery or postoperatively can improve the accuracy and speed at which finalisation can be completed.
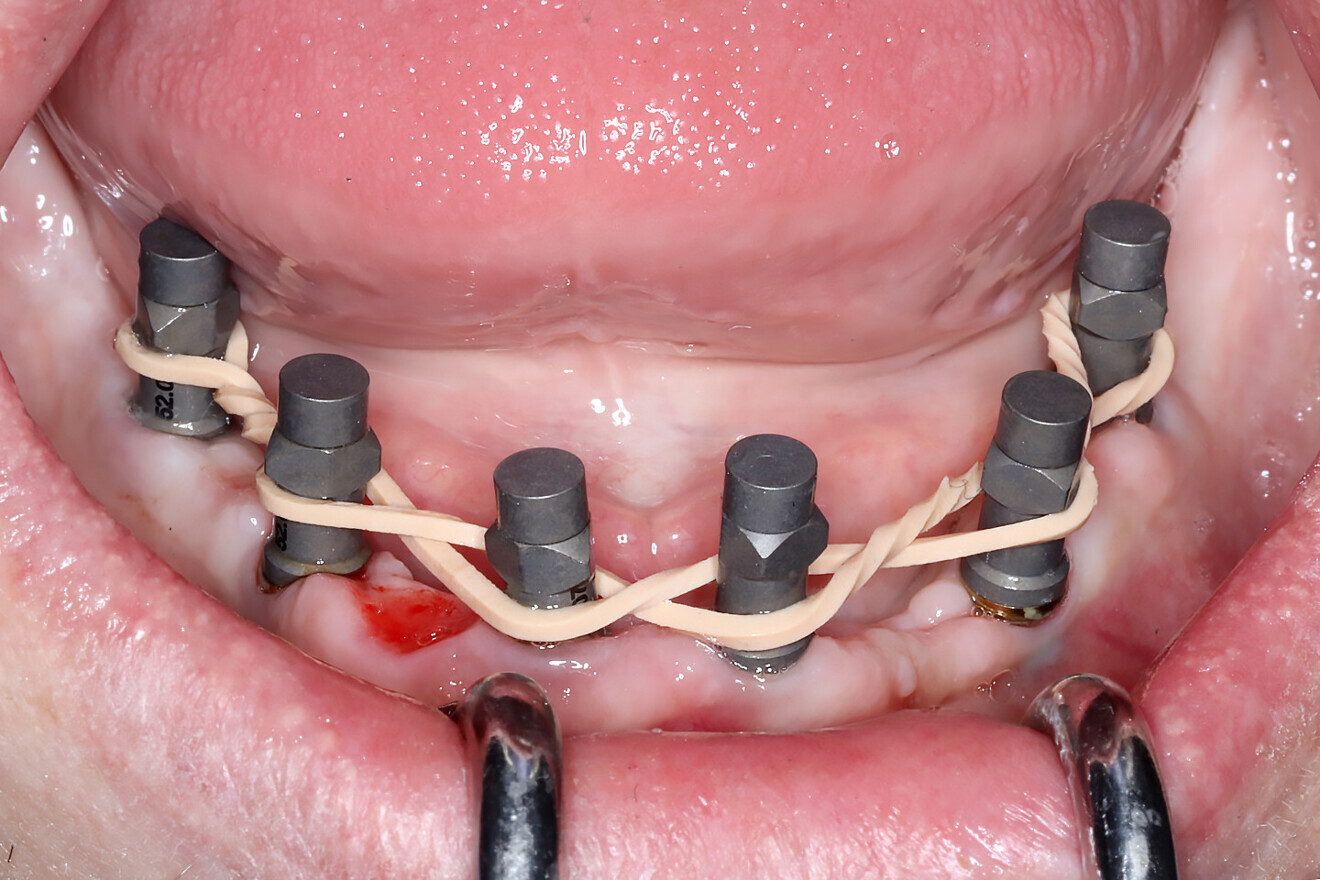
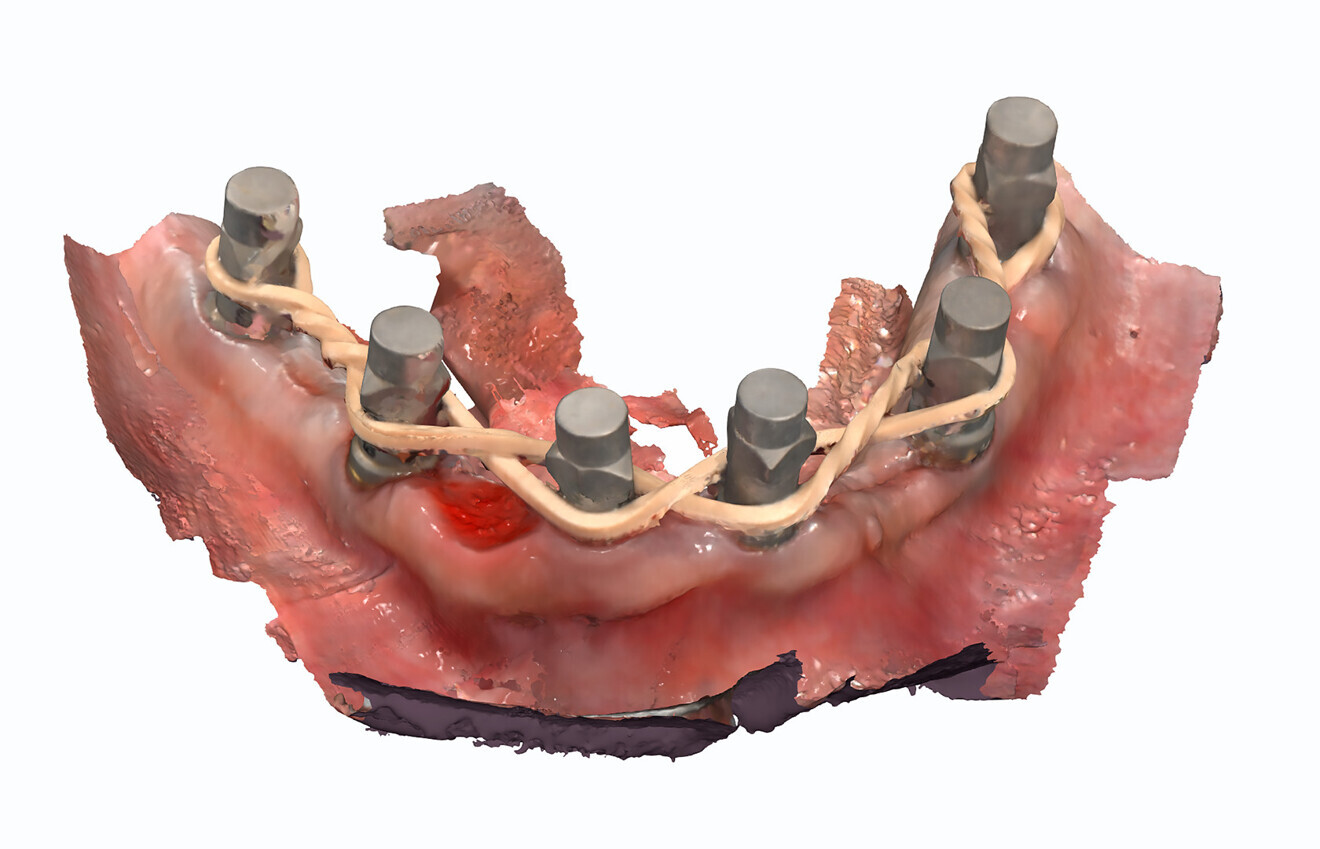
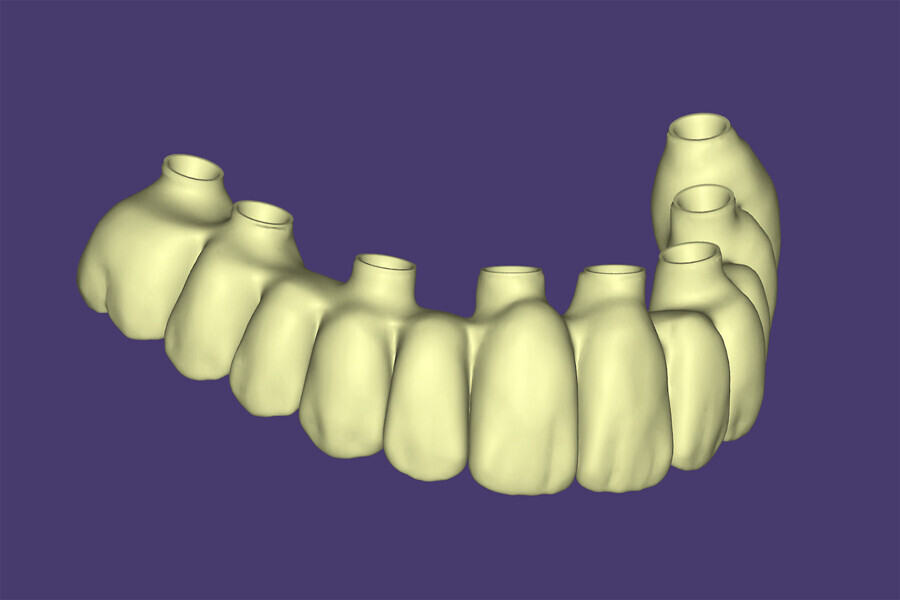
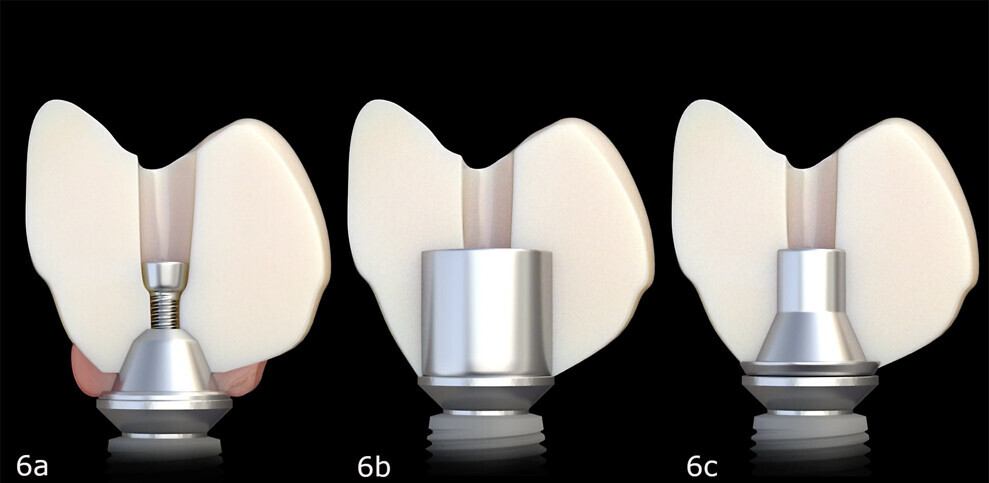
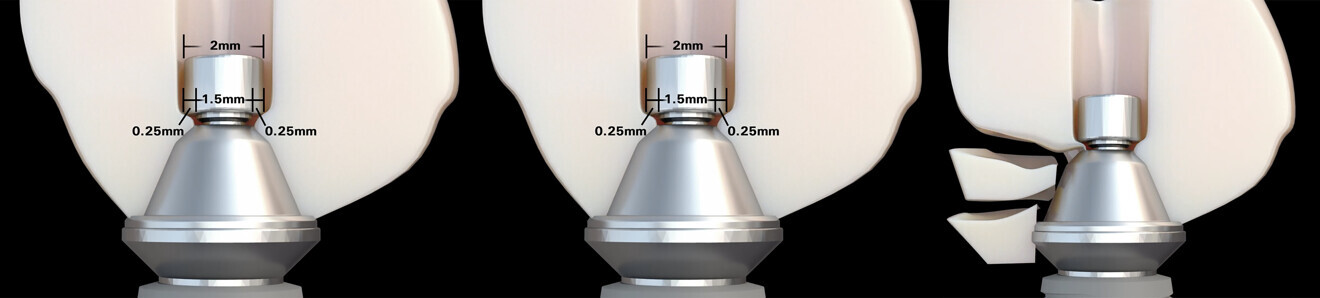
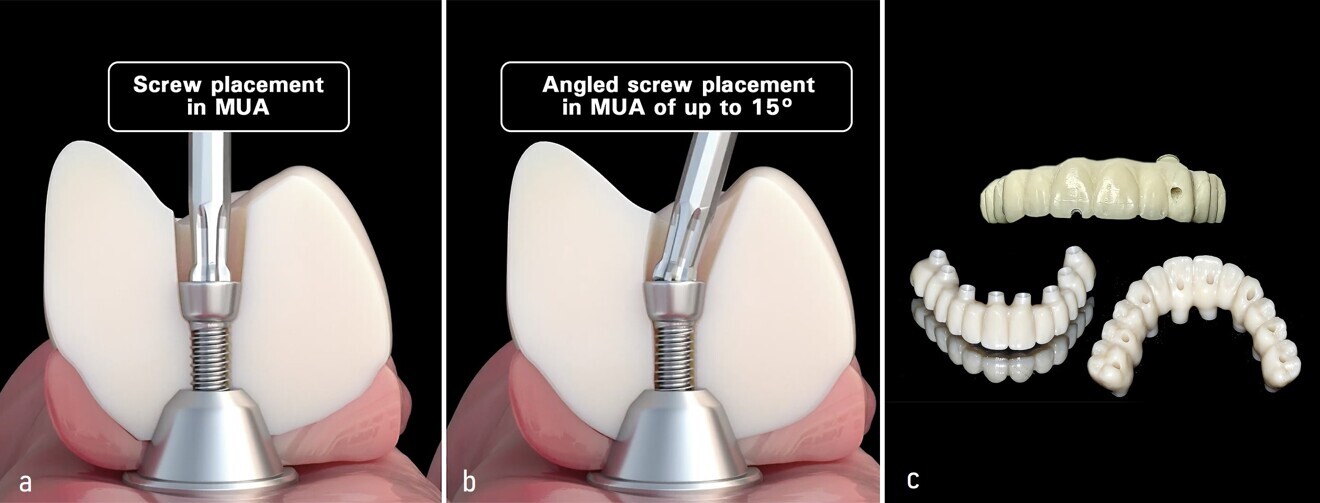
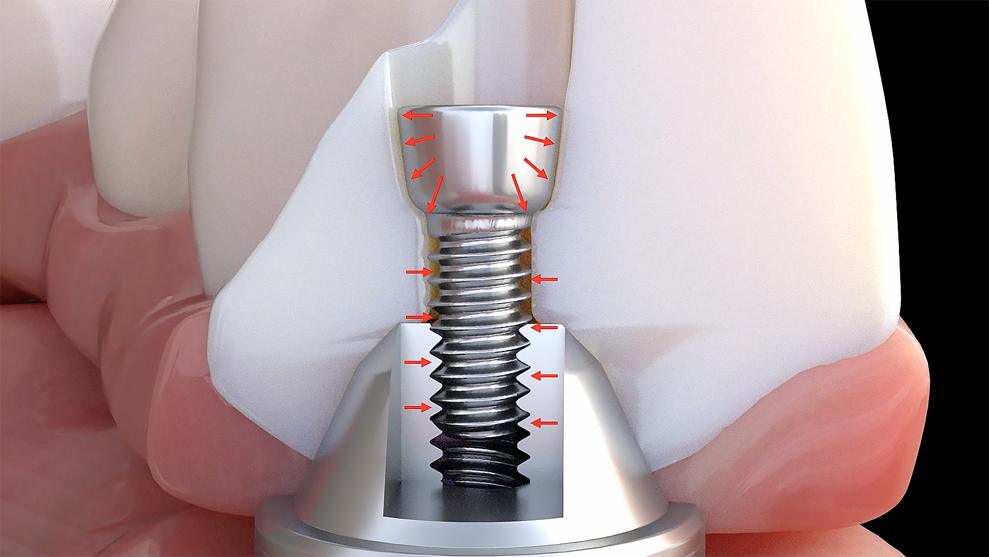
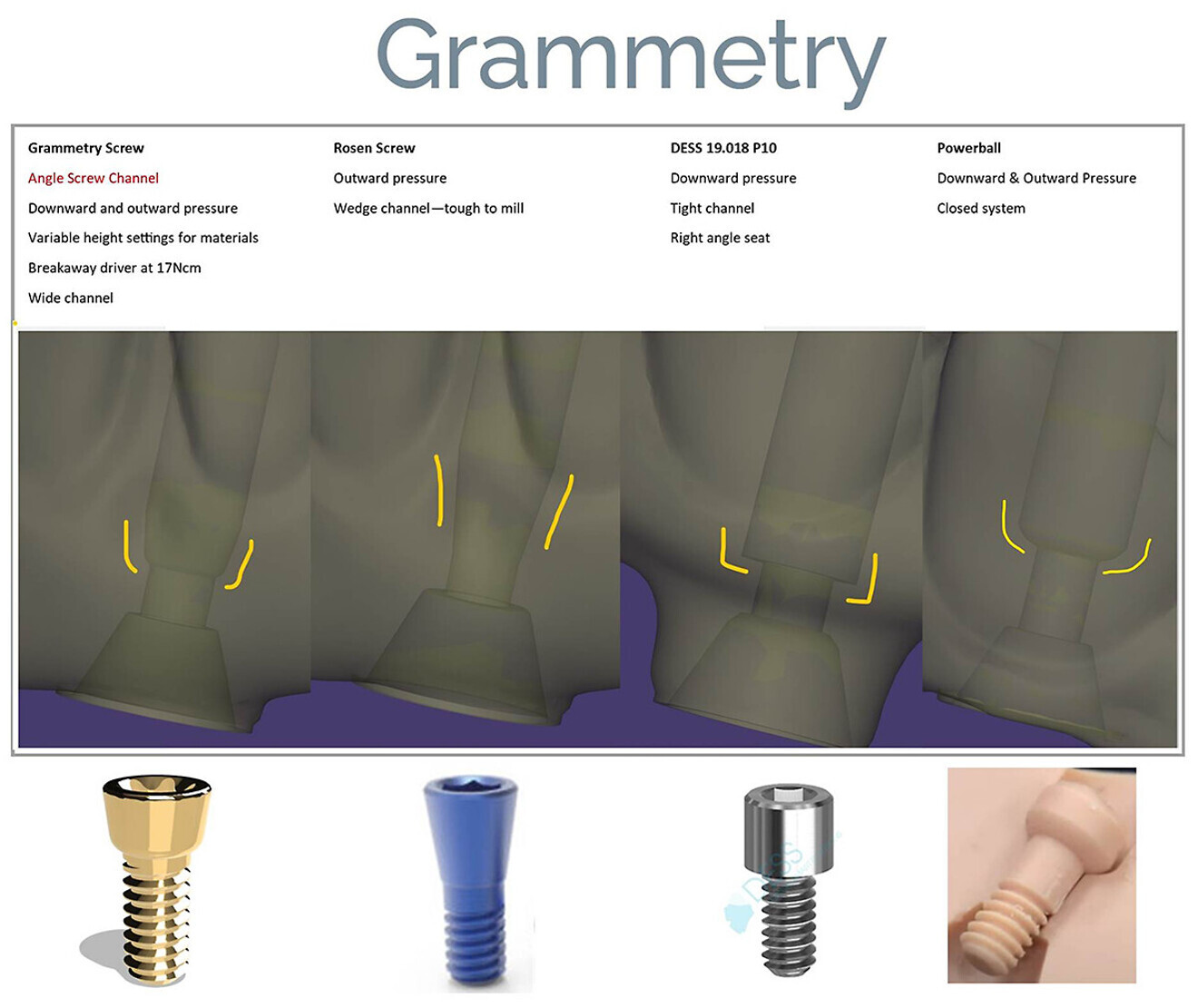
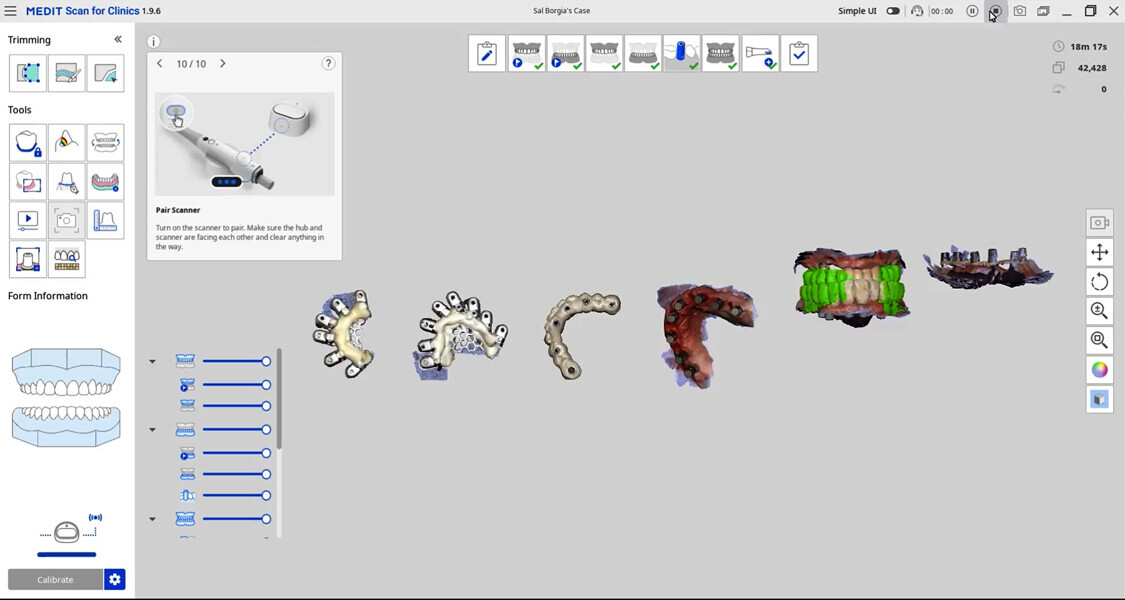
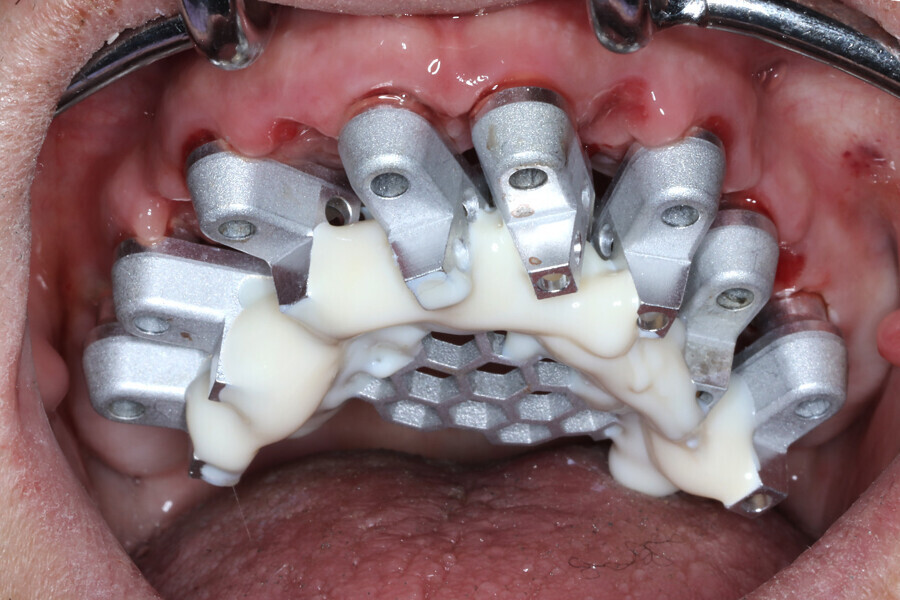
The present case described digital and analogue protocols for capturing soft-tissue topography as well as the use of iJIG provisional restorations essential to aligning and validating the intra-oral position of restorations, as well as the use of Grammetry and photogrammetry. Voids can be shown with accuracy and adjusted to be filled in using design software. With incorporation of a 2D profile photograph or, better yet, a 3D facial scan, tooth position, size and shape can be easily managed for an improved try-in or final restoration.
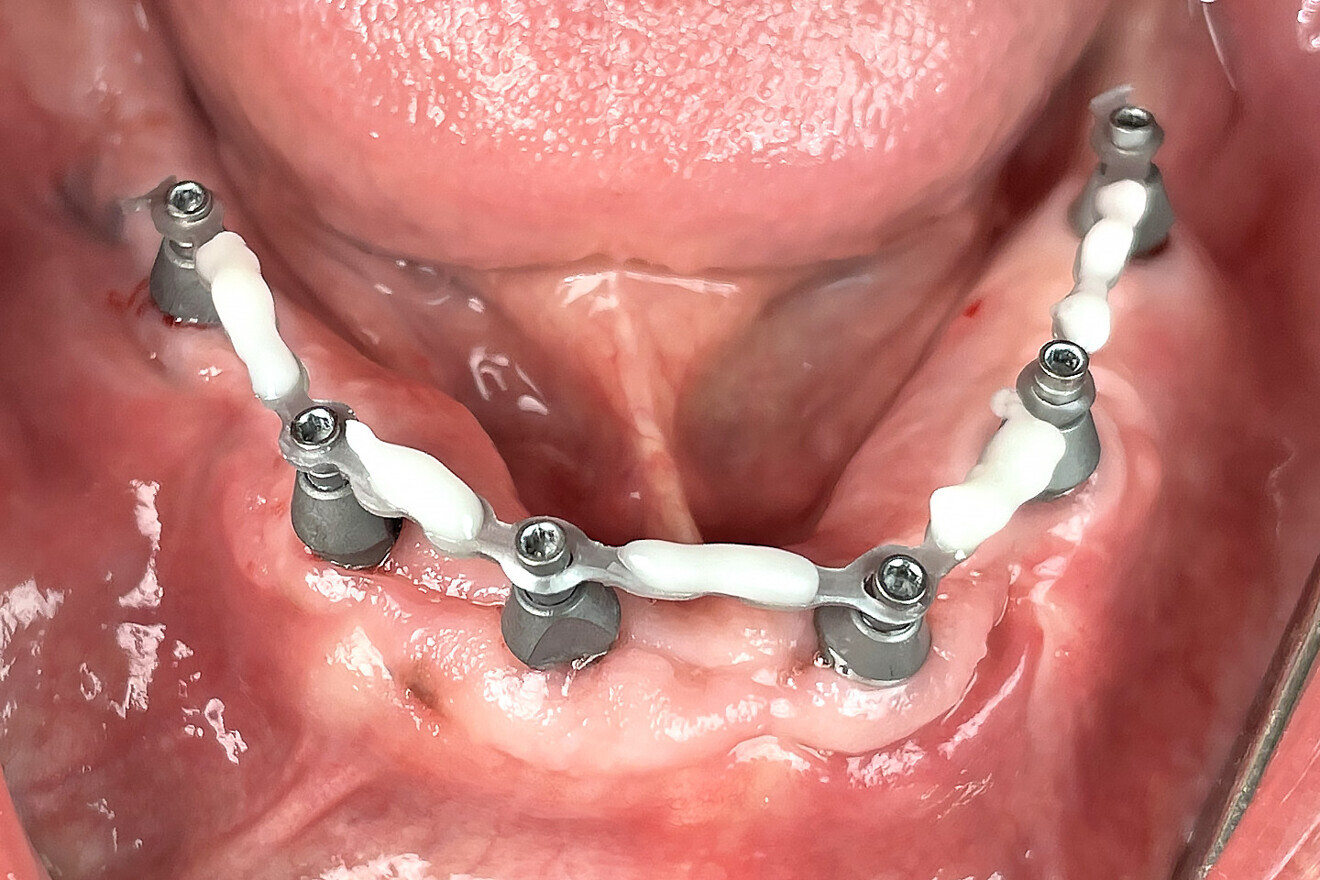
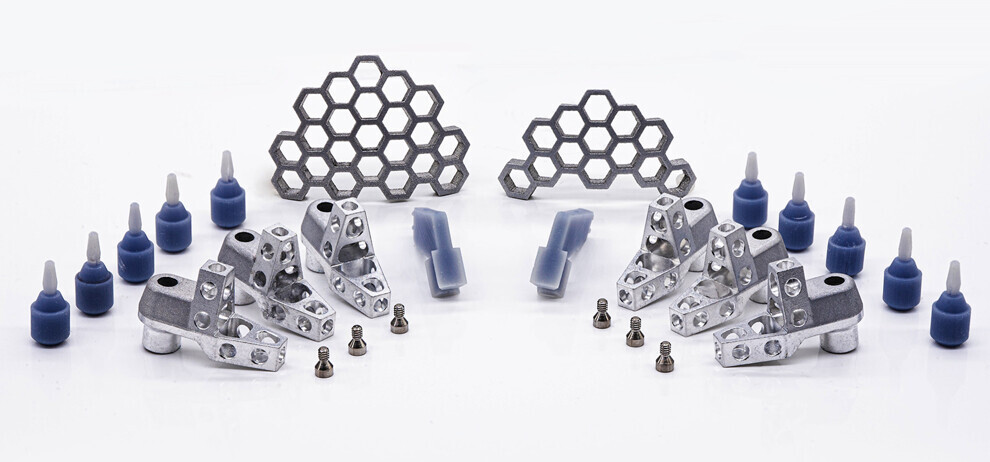
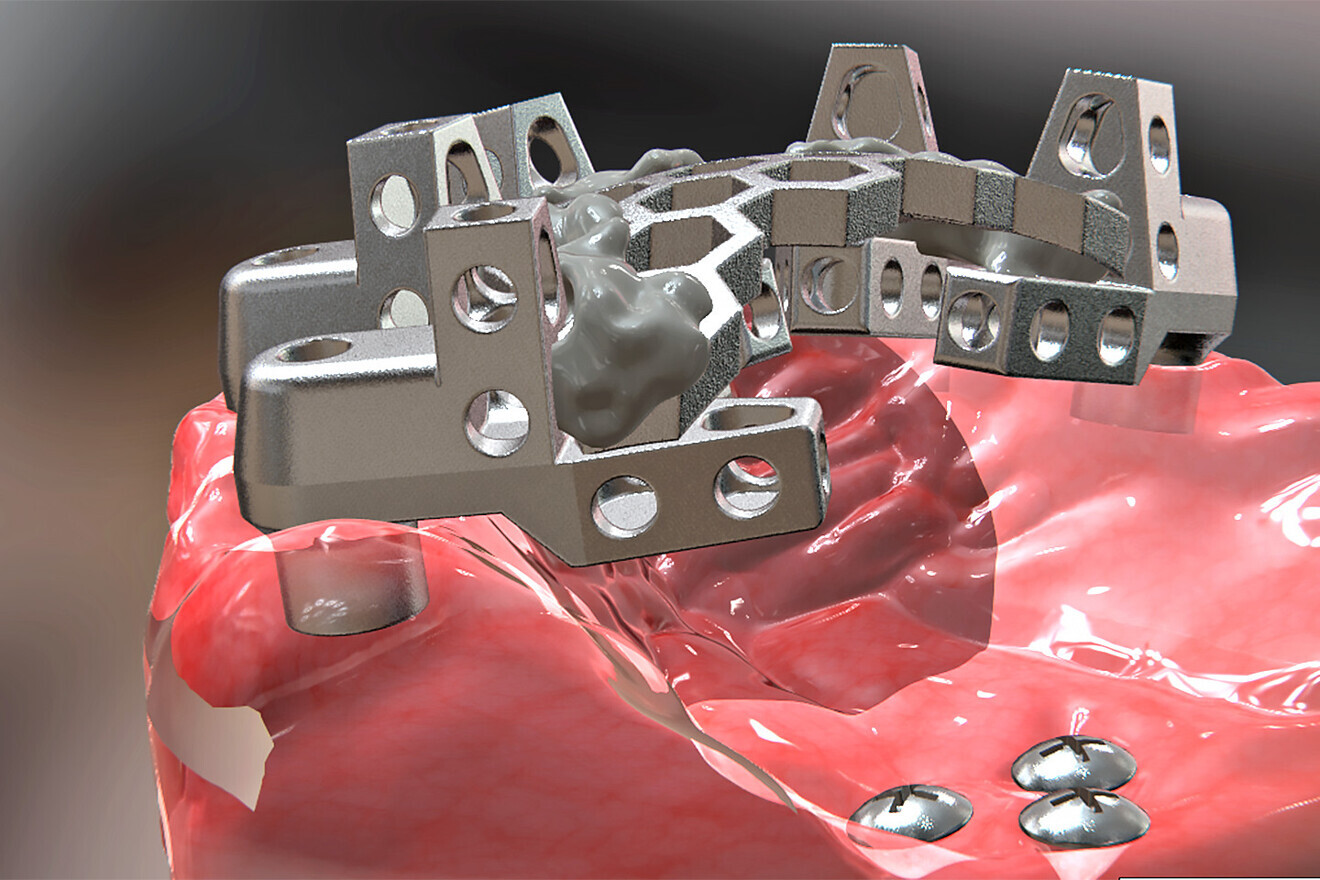
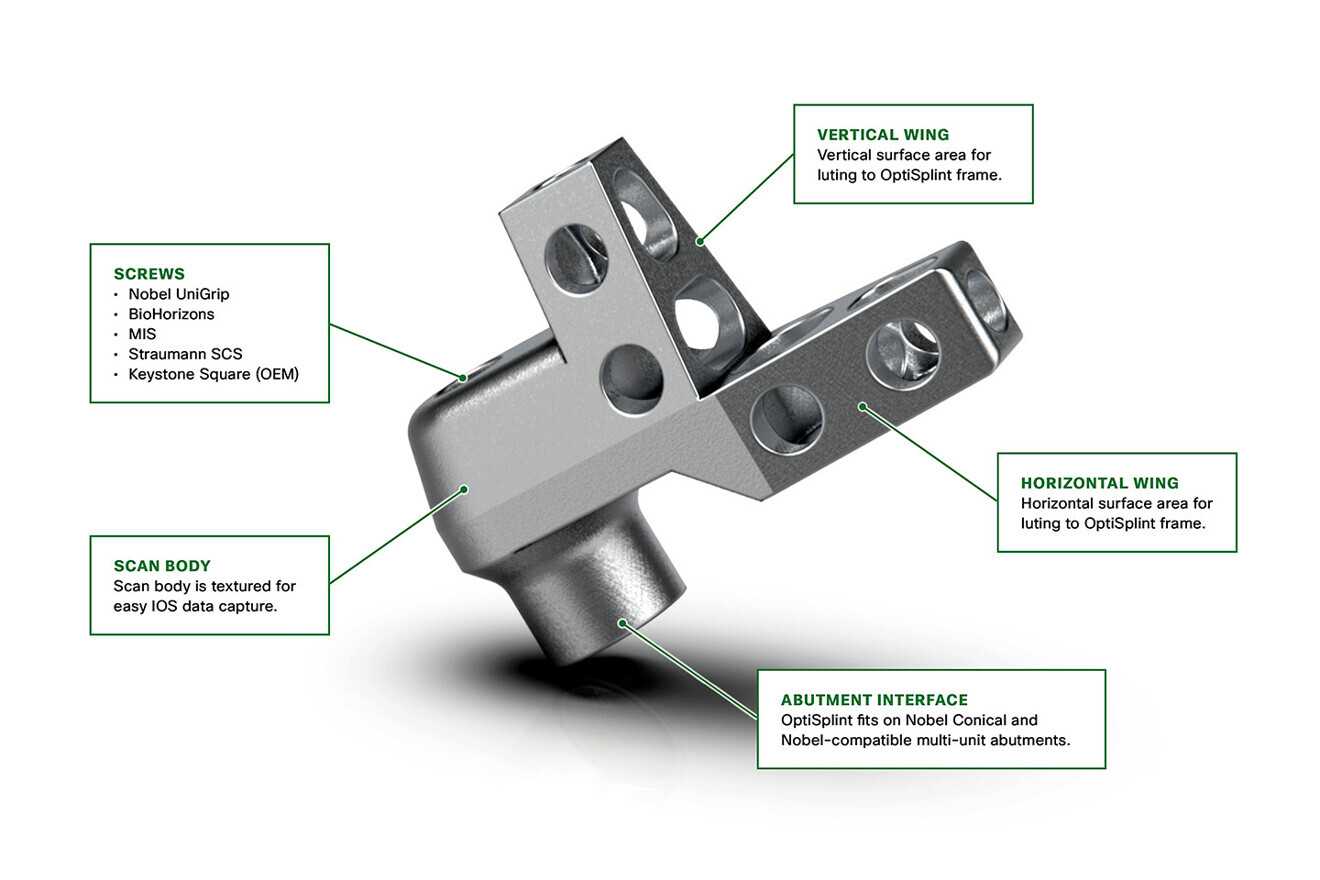
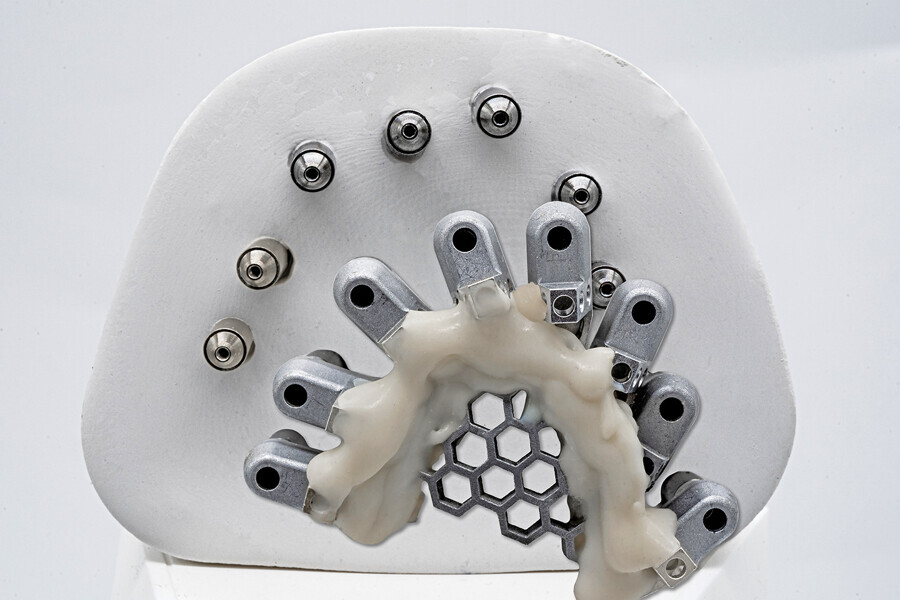
In this case, three methods were utilised to capture data to provide a basis of comparison. The first, photogrammetry, has been acknowledged as the gold standard for implant position accuracy. The second, Grammetry, utilised the new OptiSplint analogue luting protocols. The third, digital capture, utilised the Grammetry OptiSplint, in which the intra-oral scanner and extra-oral desktop captures were analysed and compared. The extra-oral desktop capture of the Grammetry OptiSplint was almost identical to the photogrammetry capture when both data sets were superimposed. The extra-oral desktop capture of the Grammetry splint yielded marginally better results than the intra-oral scan captured extra-orally. Although the results may be slightly less accurate due to the human error associated with intra-oral scanners, they were more than acceptable, as CAD/CAM unit tolerances prevent milling beyond the results obtained. An added benefit of using the Grammetry process is the possibility of producing a physical model, allowing for an analogue try-in for producing both printed try-in and final milled restorations.
In summary, there are various existing digital workflows which can be successfully utilised to achieve consistent and accurate results for full-arch implant-supported restorations. Currently, owing to supply chain shortages and limitations, photogrammetry devices are on back order and in short supply. Grammetry protocol components are both available and less expensive. For the purposes of this case presentation, it was found that the analogue–digital protocol of Grammetry can be used as an effective, affordable and equally accurate alternative to photogrammetry. In combination with the necessary records, Grammetry can provide a fully digital capture of implant positions while providing analogue models if desired for articulation and restoration fabrication. Capturing data either on the day of surgery or later on can greatly improve dental laboratory communication and reduce final prosthesis production time while supporting a high level of accuracy, enhancing the overall clinical and patient experience. Future research on the protocols and materials utilised for this case presentation is recommended, as the search for the most economical and accurate digital workflows continues to evolve.



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East






































































To post a reply please login or register