“Doctor, I was fine until I had my braces on, but now I think I have TMJ.” In every orthodontic practice, this situation arises consistently and with alarming regularity. TMJ disorder is one of the most common problems affecting millions of people each year.
Yet almost every case is not properly diagnosed or treated, causing continuous pain for the patient. This is apparent even in the orthodontic office.
Studies show that “the prevalence of TMJ signs and symptoms has been noted in several reports and ranges between 35 percent to 72 per cent.”1
If we refer to the American Journal of Orthodontics and Dentofacial Orthopedics, the majority of our orthodontic patients have signs and symptoms of TMJ disorder.1 What is the management strategy for these patients to avoid unjustified blame being placed on orthodontic treatment?
Patients and parents are more knowledgeable than ever, with Google being the new university for the general public. It becomes difficult to say TMJ disorder has nothing to do with the orthodontic treatment.
The literature is certainly inconclusive for now about the impact of diverse orthodontic techniques, with or without extractions, on the causation and treatment of TMJ disorder. We know it is out there, but what changes need to be made to our treatment techniques to avoid the focus of attention on TMJ?
In the future, the widely used cop out of, “It’s not my problem,” will be unsuccessful against a class action.
Causes and treatments are heavily debatable. There have been prominent legal cases claiming extractions were the sole cause of TMD.
For years, professionals have been treating patients with functional appliances to prevent TMJ/D. However, there are no evidence-based techniques that confirm what you do clinically every day.
Do your techniques make TMD better or potentially worse? We must find the appropriate professionals to give the clinician a better guide than at present.
This short article is in contrast to the volumes written about TMJ/craniomandibular/myofacial pain disorders, with most of them being far removed from the day-to-day issues of orthodontic practice.
If the author has one suggestion, it is that orthodontists need to be aware that full evaluation of every orthodontic patient for TMJ disorder is mandatory. Every new patient should be evaluated for his or her TMJ status and should be questioned on the presence of key symptoms, such as headaches and ear and eye pain, as well as classic TMD intracapsular symptoms.
You will be asked at some time if the patient had the symptoms before orthodontic treatment; if you have no records, you have no defense. You will need to compare this with the records during and after the orthodontic treatment. Many orthodontists do this already, but it should be a universal practice.
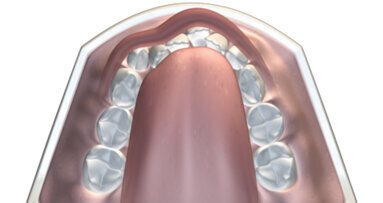
By association, the orthodontist can be drawn in to the TMJ/D issue. There is no proven link between orthodontic treatment and TMJ disorder; however, the position and function of the condyles is directly controlled by the oral structure (see illustration above). Therefore, the orthodontist’s actions can influence the TM joints. This is a question of anatomy, not law.
So why do so many of our young patients have a prevalence of TMJ disorder?
Are they experiencing an early degenerative disease, and if this is the case, why is this problem so common?
New theory of TMJ disorder—the convenient truce
Proposition 1:
- TMJ disorder is caused by trauma to the TM joints, which causes pain in the associated cranio-mandibular muscles.
- Incorrect myofunctional habits—reverse swallow, tongue thrust and mouth breathing—cause the condyles to be distalised and traumatized 2,000 times a day. The trauma to the TM joints starts at an early age and explains the high prevalence of TMD in children and adolescents.
- Incorrect myofunctional habits cause malocclusion and TMJ disorder; this is the “smoking gun” of orthodontic treatment.
To avoid unnecessary parent and patient legal issues on TMD:
- Identify any TMJ disorder signs and symptoms at the first consultation visit.
- Do a TMJ muscle and joint palpation on every new patient.
- Evaluate the TMJ risk assessment before commencing your orthodontic treatment plan.
- Have adequate TMJ/D disclaimers in your treatment plans.
- Do a soft tissue dysfunction evaluation at the first consultation and identify the real causes of the TMD. The patient with the reverse swallow and tongue thrust will undergo orthodontic treatment successfully, but without correction of these habits, TMD problems may not be resolved and symptoms could worsen.
If the malocclusion is blamed for the cause of the TMJ disorder and the pain increases during treatment, you have a problem. As we know, correcting the malocclusion does not always resolve TMJ issues.
Author into
Dr. Chris Farrell, BDS, may be contacted at info@myoresearch.com.
1. TMJ/D in children and adolescents:
Associations between occlusal characteristics and signs and symptoms of TMJ dysfunction in children and young adults. Riolo, Brandt and TenHave. Am J Orthod Dentofac Orthop 1987:92:467–77.
NEW YORK, N.Y., USA: Image Orthodontics has chosen its first three children to receive full orthodontic scholarships through Smile for a Lifetime. Smile for...
Which is better: a horse or a car? While at first it seems like this is a silly question that most can easily dismiss, this question can prompt endless ...
More than 100 years ago, and before Edward Angle, dentists realized they could move teeth into a more esthetic position by applying various mechanical ...
Crocker Ventures has acquired TMJ Implants of Golden, Colo., the leading manufacturer of implants for the treatment of temporomandibular joint (TMJ) ...
CZĘSTOCHOWA, Poland: Digital transformation in orthodontics is accelerating, and the diagnostic models generated by the orthodontic software DDP AI from ...
Benjamin Franklin once stated that an ounce of prevention is worth a pound of cure. In the case of preventive orthodontics, it can logically be stated that ...
Dr Ronni Brown is an educator, researcher and dentist who treats patients who are in vulnerable circumstances and face enormous repercussions regarding ...
SAN DIEGO, US: As cannabis use becomes more common, its health risks remain under investigation—particularly its impact on cancer. Some users develop ...
Many have now accepted The Myobrace System is peerless in terms of the potential to cajole the orofacial muscles into widening arches and allowing good ...
There have obviously been multiple impacts of COVID-19 on the human race. Measured adjustments to our normal routines, our families and how we have ...
Live webinar
Wed. 4 March 2026
12:00 PM EST (New York)
Munther Sulieman LDS RCS (Eng) BDS (Lond) MSc PhD
Live webinar
Wed. 4 March 2026
1:00 PM EST (New York)
Live webinar
Wed. 4 March 2026
8:30 PM EST (New York)
Lancette VanGuilder BS, RDH, PHEDH, CEAS, FADHA
Live webinar
Fri. 6 March 2026
3:00 AM EST (New York)
Live webinar
Mon. 9 March 2026
12:30 PM EST (New York)
Live webinar
Mon. 9 March 2026
3:00 PM EST (New York)
Live webinar
Tue. 10 March 2026
4:00 AM EST (New York)
Assoc. Prof. Aaron Davis, Prof. Sarah Baker



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 International / International
International / International
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East




















































To post a reply please login or register